OU students learn about Neonatal Abstinence Syndrome at annual workshop
Conducted virtually, OU's fifth annual Interprofessional Education Workshop focused on Neonatal Abstinence Syndrome, a condition caused when babies are exposed to opioids in the womb.
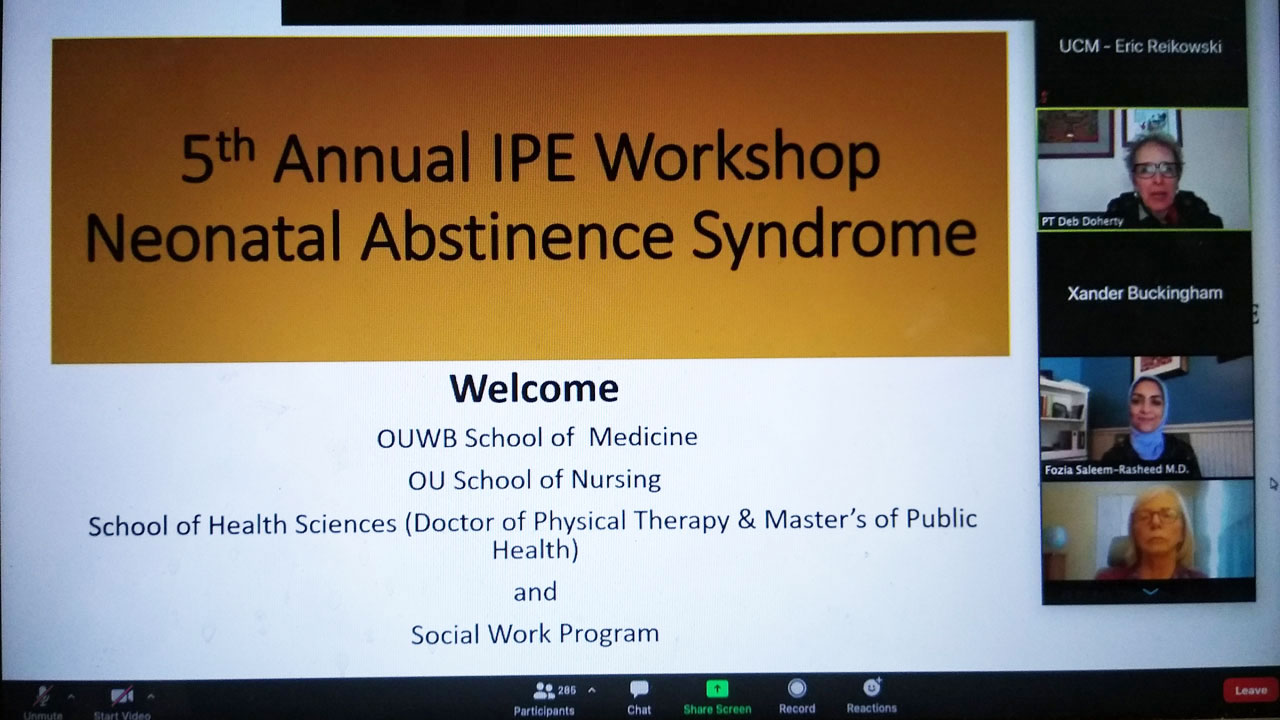
Nearly 300 students from a variety of health-oriented academic programs recently took part in Oakland University’s fifth annual Interprofessional Education Workshop on opioid abuse. Although this year’s event was held virtually due to the coronavirus pandemic, it featured plenty of insights into the challenges and opportunities health professionals have to deliver the highest quality of patient care.
This year’s event was focused on Neonatal Abstinence Syndrome (NAS), a withdrawal syndrome that can occur in newborns exposed to certain substances, including opioids, during pregnancy. NAS develops in about 50-80% of all newborns exposed to narcotics in utero and is characterized by the withdrawal symptoms (high-pitched cry, irritability, tremors, jitteriness etc.) that occur as the drugs gradually clear from the baby’s system.
“Each year, we try to find a component of the opioid crisis that also allows us to demonstrate the need for interprofessional collaboration,” said Deb Doherty, associate professor and chair of the Human Movement Science Department and the Interprofessional Education Task Force at OU. “NAS truly embodies the need for interprofessional collaboration. Our students in medicine, nursing, physical therapy, social work and public health are equally essential to the treatment of a child with NAS and their family.

Fozia Saleem-Rasheed, M.D., board-certified neonatologist at Beaumont Children's Hospital, was the keynote speaker at this year's Interprofessional Education Workshop.
The event was keynoted by Fozia Saleem-Rasheed, M.D., a board-certified neonatologist at Beaumont Children’s Hospital. She shared her experiences caring for babies with NAS and also highlighted roles and responsibilities of care team members in supporting those affected by the condition.
“It takes a multidisciplinary team to make sure the needs of each neonate and parent are addressed,” Dr. Saleem-Rasheed said. “The mainstay of treatment is optimizing nonpharmacological interventions and the multidisciplinary team is key in doing that.”
The care team includes neonatologists, residents, nurse practitioners, nurses and nursing managers, social workers, pharmacists and physical therapists. Each specialty contributes to the care plan, which involves not only medical interventions, but psychosocial support as well.
“There’s always a history for why parents are on opioids,” Dr. Saleem-Rasheed said. “It’s a complex history that we need to recognize. Parents often feel a lot of anxiety, shame and guilt, and also a fear of being judged by the medical team or other family members.”
She added that it’s important to be able to “withhold judgment and have compassion” for patients and family members regardless of their personal circumstances and empower them to be a part of the baby’s care.

Participants discussed a case study during the workshop.
Following the keynote, students gathered in small teams to discuss a case study involving an infant and mother dealing with NAS and related issues. Each group was led by a faculty facilitator and a student facilitator who helped guide the discussion.
Later, the case study was discussed by a panel of health professionals who highlighted multi-disciplinary intervention options to limit the use of prescription opioids. The panel was moderated by Stephen Loftus, Ph.D., OUWB associate professor of medical education and included five health professionals:
- Kristen Brown, LLMSW, Clinical Social Worker
- Veena Rajanna, MS, PharmD, BCPS, BCPPS, Clinical Pharmacy Specialist
- Robin Blalock, MPT, Physical Therapist
- Amy Gaither, RN
- Halli Rennaker, BS, Project Coordinator, Michigan Public Health Institute

 February 12, 2021
February 12, 2021